One Mistake, Multiple Consequences: Pre-Analytical Risk in Pathology
By Dr. Amar S. Bhogal
Doctors and clinicians depend on the reliability and accuracy of laboratory results when investigating patients with undiagnosed symptoms. We base critical decisions, treatments, and emergency interventions on these findings. Yet, I frequently witness alarming errors: abnormally high potassium values that prompt urgent action, only to normalise on repeat testing, or results returned that belong to an entirely different patient. These aren’t minor glitches in the system; they expose the fragility of the pre-analytical phase in laboratory diagnostics.
The pre-analytical phase covers every step before analysis. It starts with the test request and includes order entry, patient identification, sample collection (phlebotomy), labelling, handling, and transport. This stage is particularly vulnerable to human error. Even simple missteps in blood draw technique, patient verification, tube selection, or transport timing can skew results or lead to misdiagnoses.
In some hospitals, phlebotomists print the blood tube labels centrally and then try to match with the patients on their phlebotomy ward round. And not surprisingly, they get it wrong ~1% of the time – meaning the wrong results assigned to a patient. Let’s consider the impact of an error rate of just 0.6%, observed in one hospital studied. For a teaching hospital with 1000 beds that bleeds 300 patients every day, this means at least two incorrect results every day or ~800 incorrect results per year. If 5% of these tests are critical – by which we mean a missed severe hyperkalaemia, new onset acute kidney injury or evidence of worsening infection – then each year we can estimate that around 40 patients are harmed. A good solution is to scan the patient’s wristband and print container labels at the bedside Then, scan the tubes when taken so that such errors never happen.
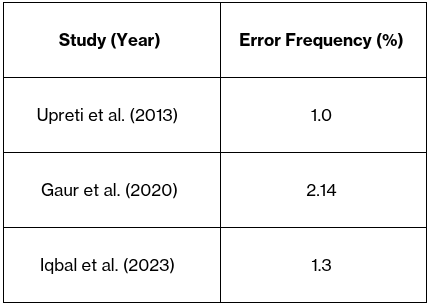
Data consistently show that most laboratory errors occur during this phase [1,2]. Several studies have shown 17-25% rates of haemolysis in samples collected in the Emergency Room or Accident and Emergency departments. For inpatients, the rate of haemolysis varies between 4.5% to 10%. These rates are unacceptable since there are measures that can reduce the rate of haemolysis through better training. But most systems deployed have no means of identifying the phlebotomist. Salutare ONE Testing identifies every person involved from who place the order, who printed the label and when, who took the blood and when, and when did the sample arrive in the laboratory. In a tertiary hospital, the pre-analytical error-rate was 1.3% with sample specific issues; clotting, haemolysis, and both insufficient and excess sample volumes being the greatest cause (>75%) [3]. Inappropriate tube for analysis (12%) and labelling errors (3%) were the other common errors in this critical pre-analytical phase [3]. In a haematology-focused study, misidentification caused 0.35% of errors, while clotted and haemolysed samples added significantly to the total discrepancies [4]. Error rates across these studies highlight the issues hospitals. This waste and need for resampling carry financial strain, waste hospital and human resources, and most importantly have negative consequences on the patient (Table 1).
Table 1. Pre-Analytical Error rates across various studies
A College of American Pathologists study found that over 70% of lab-related errors arise before samples reach the lab [5]. These include inaccurate order entries, missing or incorrect labels, and substandard specimen collection techniques. Particularly troubling are “false critical results,” such as pseudo-hyperkalaemia—where improperly collected haemolysed specimens falsely elevate potassium levels and trigger unnecessary interventions [6].
To tackle this, Barak and Jaschek highlighted IT drive measures, such as barcoded tubes, centralised LIS integration, and automated clinical-to-lab data transfer. Their approach reduced pre-analytical errors from 2.7% to 0.77% across millions of tests [1]. With the average cost of pre-analytical errors standing at $208 in the US, this reduction although small, can mean huge financial savings for hospitals [7]. Chawla et al. reinforced the need for rigorous staff training, detailed standard operating procedures (SOPs), and comprehensive phlebotomy education to minimise haemolysis and sample rejection [3].
Despite these advances, many healthcare systems still depend on paper forms, handwritten labels, and fragmented communication between clinical and lab teams. This disconnect leaves dangerous gaps in patient care.
Bridging the Gap: How Digital Solutions Transform Sample Integrity
Salutare ONE Testing offers a simple and safe way forward. Digital blood forms, pre-labelled tubes, and intelligent de-duplication systems transform the pre-analytical process into a streamlined, error-resistant chain. By minimising human error, ONE Testing delivers safer, faster, and more accurate diagnostics. Exactly what modern healthcare demands [8].
References
Barak M, Jaschek R. A new and effective way for preventing pre-analytical laboratory errors. Clin Chem Lab Med. 2014;52(2):e5-e8. doi:10.1515/cclm-2013-0597.
Carraro P, Plebani M. Errors in a stat laboratory: types and frequencies 10 years later. Clin Chem. 2007;53(7):1338-42.
Iqbal MS, Tabassum A, Arbaeen AF, Qasem AH, Elshemi AG, Almasmoum H. Preanalytical Errors in a Hematology Laboratory: An Experience from a Tertiary Care Center. Diagnostics (Basel). 2023 Feb 6;13(4):591. doi:10.3390/diagnostics13040591. PubMed PMID: 36832079; PMCID: PMC9955620.
Upreti S, Upreti S, Bansal R, et al. Types and frequency of preanalytical errors in haematology lab. J Clin Diagn Res. 2013;7(11):2491-3. doi:10.7860/JCDR/2013/6399.3587.
Valenstein PN, Raab SS, Walsh MK. Identification errors involving clinical laboratories: a College of American Pathologists Q-Probes study. Arch Pathol Lab Med. 2006;130(8):1106-13.
Lippi G, Plebani M, Di Somma S, Cervellin G. Hemolyzed specimens: a major challenge for emergency departments and clinical laboratories. Crit Rev Clin Lab Sci. 2011;48(3):143-53. doi:10.3109/10408363.2011.576312.
Green SF. The cost of poor blood specimen quality and errors in preanalytical processes. Clin Biochem. 2013;46(13-14):1175-1179.
Salutare. ONE Testing. Available from: https://www.salutare.co.uk/solutions.
Gaur K, Puri V, Shukla S, Sharma S, Suman S, Singh R. Finish before the start: Analyzing preanalytical sample errors in a tertiary care hematology laboratory. Indian J Pathol Microbiol. 2020 Jul‑Sep;63(3):435–440. doi:10.4103/IJPM.IJPM_191_19. PubMed PMID: 32769334.
J Emerg Nurs. 2023 Jan;49(1):134-139. doi: 10.1016/j.jen.2022.08.005. Epub 2022 Sep 20.
J Emerg Nurs. 2023 Sept;49(5):744-754; doi: 10.1016/j.jen.2023.06.001
Arch Pathol Lab Med (2018) 142(2):229-235; doi: 10.5858/arpa.2016-0400-OA
About the Author
Dr. Amar S. Bhogal is a junior doctor in the United Kingdom, dedicated to enhancing patient outcomes through the integration of advanced healthcare technologies. He has a robust background in medical research, having served as a Research Assistant at University College London's Institute for Liver and Digestive Health. His work has been pivotal in exploring the application of remote technology to support acute inpatient and transitional care, particularly for individuals with chronic obstructive pulmonary disease (COPD).
Beyond clinical medicine, Dr. Bhogal has held leadership roles in both the publishing and education sectors. He worked with Elsevier as a commissioning and managing editor for oncology journals, playing a key role in curating and advancing high-impact scientific research. Additionally, he served as a director for an educational startup focused on supporting children from disadvantaged backgrounds, demonstrating his commitment to widening access to education and fostering opportunities for young learners.
Passionate about the transformative potential of healthcare technologies, Dr. Bhogal is focused on leveraging innovative solutions to improve clinical practices and patient care.
Time to be healthcareful®